Beyond the quick fixes of medications are the causes that lie beneath their need. Addressing health care from a holistic perspective must precede the Rx pad.
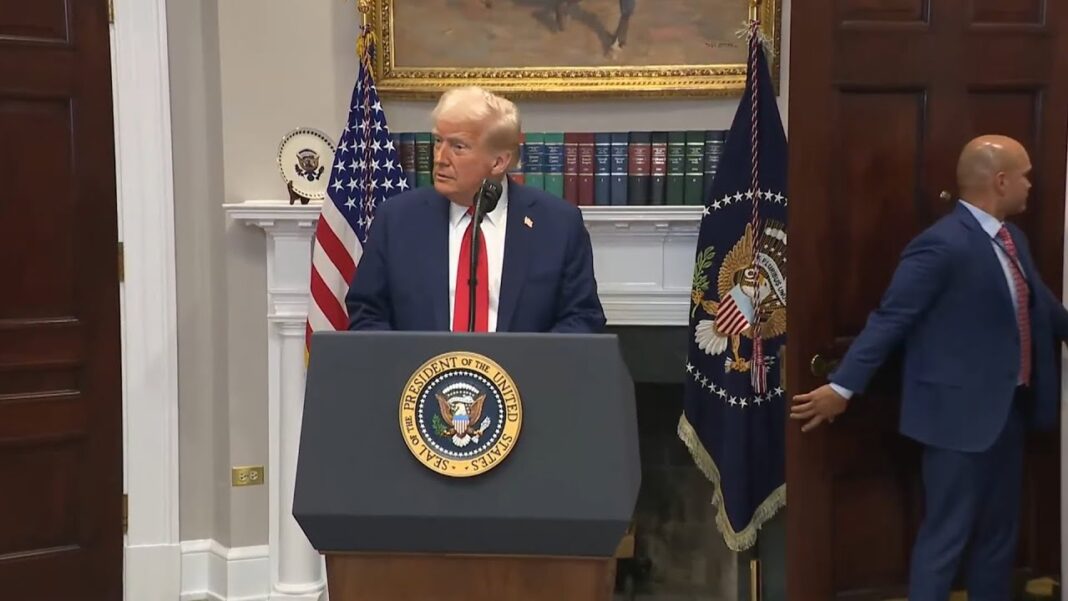
President Donald Trump’s revived effort to reduce prescription drug prices is a long-overdue step toward affordability. For millions of Americans, the cost of staying alive has become burdensome, and any policy that eases the burden is worth celebrating.
However, as a physician, I’ve seen what happens when medications become too cheap, plentiful, and automatic. If we don’t reform how drugs are used, we risk trading financial hardship for clinical harm.
Vagaries of Lower Drug Costs
In today’s health care system, medication is the first answer—and often the last, especially for older adults. More than 40 percent of those over 65 take five or more prescriptions daily, nearly double the 24 percent prevalence observed between 1999 and 2000.
The reliance on medications isn’t comprehensive care—it’s chemical accumulation. Fatigue, confusion, and chronic adverse effects are often misread as new illnesses, triggering more prescriptions.
A telling example is a 60-year-old woman who came to my clinic drained of energy and hope. She had been prescribed antidepressants and sleep aids, though her problem wasn’t mental. A sleep study revealed severe sleep apnea, which was fragmenting her rest and destabilizing her blood sugar. Beneath her surface, symptoms were years of suppressed grief and emotional exhaustion. With blood sugar support, trauma integration, and reconnection to her values, she got her life back, without adding another prescription. There is a path forward, without reliance on medications.
‘Following Directions’ Could Be Deadly
Most people assume medication harm results from misuse. However, a more insidious danger is adverse drug events (ADEs)—when harm occurs even though the drug was taken correctly.
As of 2025, ADEs account for more than 250,000 deaths annually, becoming the third leading cause of death in the United States—just behind heart disease and cancer—according to an analysis by the American Society of Pharmacovigilance. ADEs are outranking conditions such as stroke, diabetes, and Alzheimer’s disease. These are deaths from medications working exactly as designed, but in bodies that couldn’t sustain the chemical load.
The ASP report notes, “With better tools and more accurate reporting, many of these deaths could be prevented. Until then, we are left with a sobering truth: the medicines we rely on to save lives may, in far too many cases, be taking them.”
By Jingduan Yang, M.D