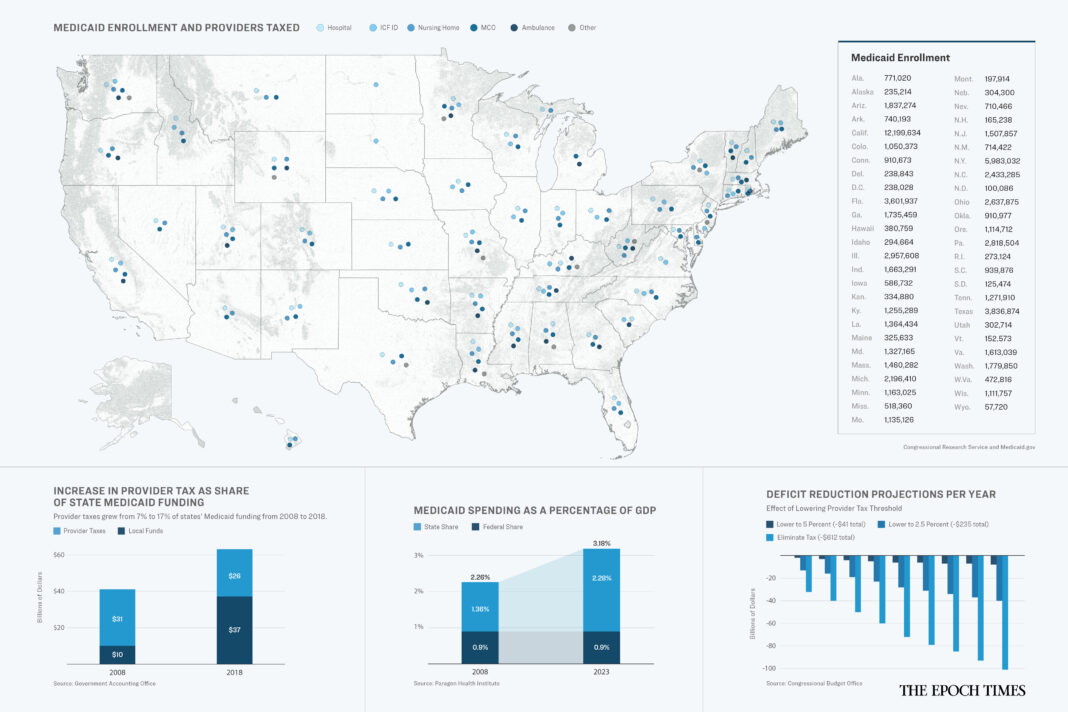
How states inflate the cost of Medicaid to get more money from the federal treasury.
Medicaid is a broadly popular program that provides medical coverage to low-income Americans through a combination of state and federal funding. More than 60 percent of Americans either know someone who has benefited from Medicaid or have been enrolled themselves, according to health policy think tank FFF. So any talk of altering the program usually meets strong opposition.
Yet few seem to know how the system works, what it costs, or the level of unnecessary spending hidden within its $880 billion annual budget.
One example is a little-known quirk in the Medicaid system that allows states to artificially inflate their Medicaid costs to recoup more federal dollars. The arrangement allows some states to pocket a share of the money paid to them for providing treatment to Medicaid patients.
Here’s how it works.
The Loophole
When a Medicaid patient receives a treatment or service, the state pays the doctor, hospital, nursing home, or other provider. The federal government reimburses each state for a portion of its Medicaid expenses. The reimbursement ranges from 50 to 76.9 percent depending on the income level in the state and other factors.
Although, for people who enrolled through the Medicaid expansion under the Affordable Care Act, the reimbursement rate is 90 percent.
So if a state had a 60 percent reimbursement rate and spent $10 billion on Medicaid services, the federal government would reimburse the state $6 billion.
That’s how the system was designed to work back in 1965, generally speaking.
By the mid-1980s, some states had found a way to increase payments to providers and their own Medicaid costs at the expense of the federal government.
First, medical providers would either voluntarily donate money to a state or agree to pay a tax. The states would then return the amount of the donation or tax, and possibly even more, through increased reimbursement. Finally, the states would bill the federal government for the increased cost.
In some cases, the providers initiated these arrangements, according to the Congressional Research Service (CRS).