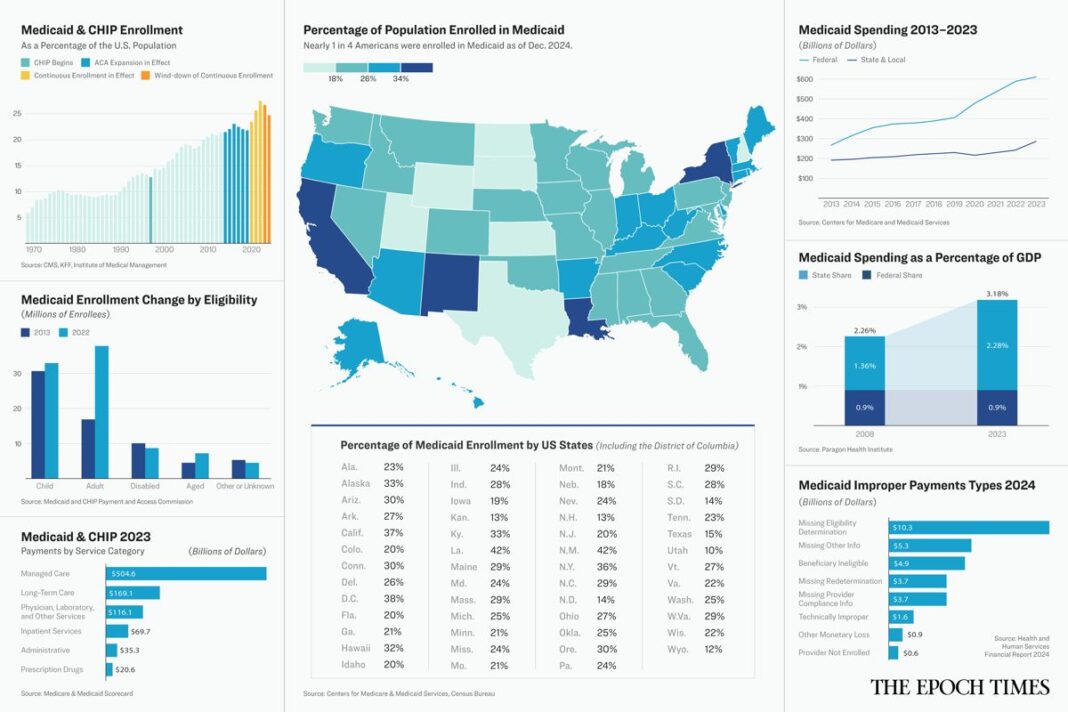
Medicaid serves nearly a quarter of the U.S. population, yet few know how it works. Here are the basics.
Medicaid, the state and federal program that provides health coverage for millions of low-income Americans, has taken center stage in Congress’s bid to pass President Donald Trump’s sweeping agenda.
In simplest terms, Republicans want to reduce the cost of the $816 billion program as part of a long-term plan to cut federal spending and implement Trump’s tax cuts and his border and energy measures.
Democrats adamantly oppose cuts to the program.
Though nearly one in four Americans is covered by Medicaid, many people seem to know little about the program or how it works.
Here are the basics of this complex system, which was created in 1965 and has been altered several times since.
What Is Medicaid?
Medicaid is a program that provides health coverage for lower-income Americans, underwritten by state and federal tax dollars. About 85 million people were enrolled in the program as of December 2024.
Medicaid is operated by the states but overseen by the federal government. No state is required to participate in Medicaid, though all states have chosen to do so.
The Centers for Medicare and Medicaid Services oversees the program on the federal level, but each state has its own Medicaid office. Some states refer to Medicaid by a different name. In California, it’s known as Medi-Cal. In Oklahoma, Medicaid is called SoonerCare.
Medicaid is not the same as the Children’s Health Insurance Program, usually called CHIP. However, the two are similar and are usually considered together.
CHIP was started in 1997 to cover medical costs for uninsured children and pregnant women whose income is too high to qualify for Medicaid but who still have trouble affording health insurance.
Who Can Get Medicaid?
Original Medicaid covers low-income people in certain categories including children, pregnant women, parents of dependent children, the elderly, and people with disabilities.
The Affordable Care Act (ACA) expanded Medicaid eligibility in 2014 to include most people who are under age 65 and who earn at or below 133 percent of the federal poverty line. That’s about $22,000 for an individual or about $42,000 for a family of four including two children.
Forty states and the District of Columbia have chosen to provide this expanded coverage.
The income threshold for CHIP eligibility varies by state and ranges from 170 percent to 400 percent of the federal poverty line.
Medicaid enrollment grew to a high of 94.6 million in April 2023 when states were required to maintain the “continuous enrollment” of nearly all Medicaid beneficiaries during COVID-19 regardless of their eligibility status. Under the Families First Coronavirus Response Act of 2020, Medicaid coverage could not be discontinued unless the enrollee requested it, moved out of state, or died.
That provision expired in March 2023, but due to the large backlog of eligibility recertifications to be processed, states have had some flexibility in winding down their continuous enrollment. The deadline for all states to comply with Medicaid and CHIP eligibility requirements is Dec. 31, 2026.